What is radiation therapy?
Radiation therapy is the medical use of high dose radiation to destroy cancer cells. Radiation is a type of energy that is produced naturally by the sun, earth, and rocks, and artificially by machines. Radiation is used for diagnostic as well as therapeutic purposes. Low dose radiation, for example, is used to take X-rays.
Cancer cells grow and divide faster than most normal cells. Radiation therapy works by damaging the cells’ DNA to interfere with cell replication and kill them. In this way, radiation can either shrink a tumour or completely destroy it.
When is radiation therapy used?
Depending on the type of tumour, radiation therapy may be used on its own or in combination with other treatments, such as surgery or chemotherapy. It is most effective with tumours that have rapidly dividing cells. Not all tumours are responsive to radiation. There are several types of tumours that can be treated with radiation therapy alone like nasal and brain tumours.
How is radiation therapy administered?
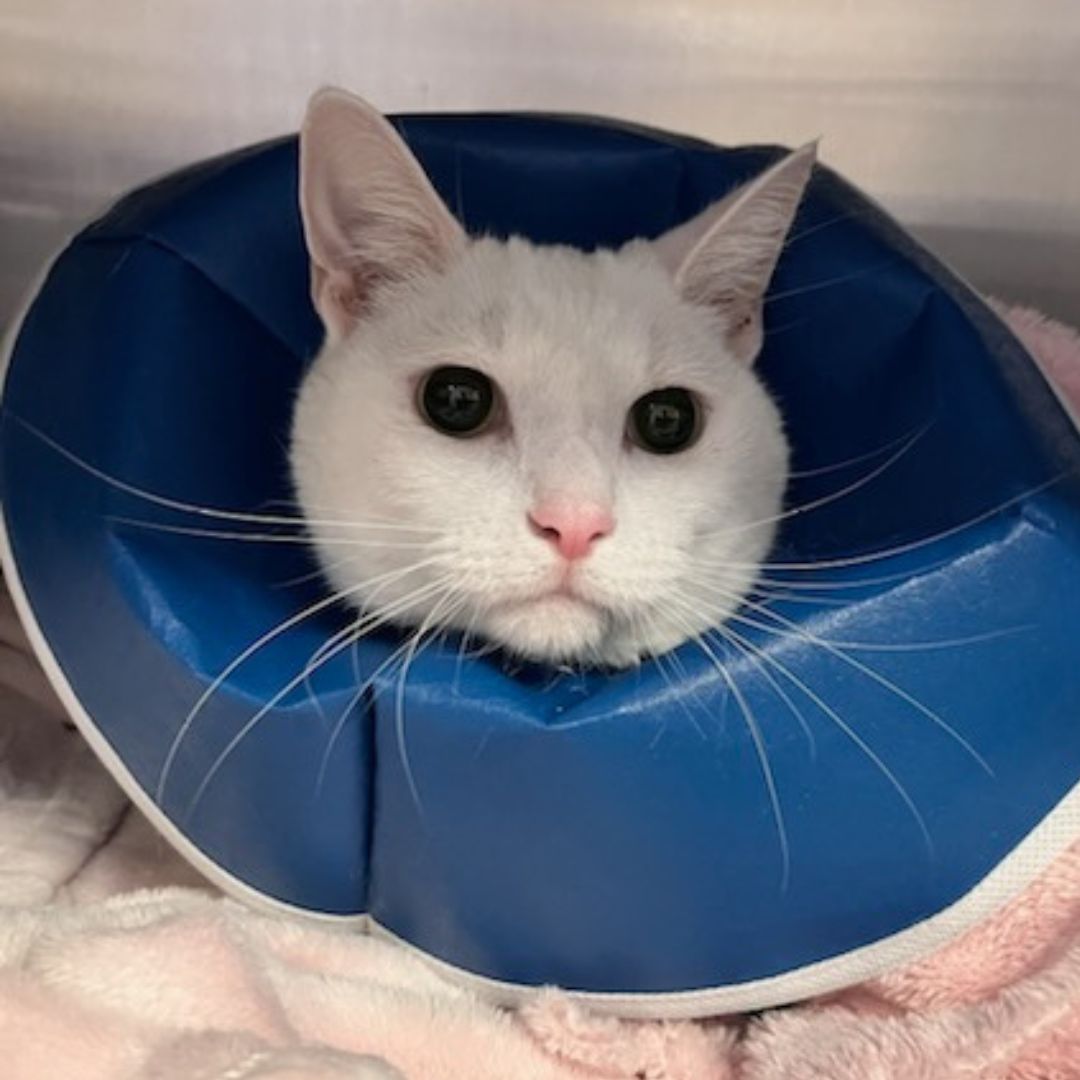
Radiation therapy is typically administered while the pet is under a general anaesthesia; the pet must be able to be placed in a reproducible position and remain completely still to allow the radiation to be delivered with absolute precision. Depending on the treatment program, your pet may need to undergo 4-5 anaesthetics. The delivery of radiation, however, is usually quick, meaning your pet will only need to spend a brief amount of time under full anaesthesia for each treatment.
Prior to commencing therapy, a planning CT scan is performed to ’mark’ the tumour location. This allows the radiation to be delivered in a focused manner, minimising damage to the surrounding normal tissues.
Stereotactic radiation therapy (SRT) involves much higher doses of radiation over the course of a few days and is better able to exclude the surrounding normal tissues than conventional radiation therapy. Although side effects are still possible, the protocol is significantly shorter.
When is radiation therapy used?
Depending on the type of tumour, radiation therapy may be used on its own or in combination with other treatments, such as surgery or chemotherapy. It is most effective with tumours that have rapidly dividing cells. Not all tumours are responsive to radiation. There are several types of tumours that can be treated with radiation therapy alone like nasal and brain tumours.
What are the side effects of radiation therapy?
The side effects of radiation therapy can be split into two broad categories: early and late effects.
Early side effects are usually observed within two weeks after starting radiation therapy and can continue up until one month after the treatment has begun. These effects are usually inflammatory, with areas such as the skin and mucous membranes being the most commonly affected. Redness, irritation, and ulceration of the treated surface can develop.
The early side effects are dependent on the tumour, its location, and the surrounding tissues that may be involved. Some other possible effects are described below:
- Delayed hair regrowth and/or regrowth of a different colour. If dark-coloured, it may be much lighter (even completely white); if light-coloured, it may be much darker.
- If the mouth is being treated, side effects can include excessive salivation, bad breath (halitosis), formation of plaques or ulcers, and secondary infections.
- If the eye is being treated, side effects such as blepharitis, conjunctivitis, and keratitis (inflammation of the eyelids, surface of the eye, and cornea respectively) are possible. The eye can become dry due to a change in normal tear production and is susceptible to corneal ulceration (an open sore on the cornea). Cataracts and retinal damage are also possible and may lead to loss of vision.
- If the intestinal tract is within the radiation field, diarrhoea may also be observed.
Late side effects usually occur more than six months after therapy. These effects are also dependent on the tumour and the surrounding tissues that may be involved.
Contributors: Debbie Stoewen DVM, MSW, RSW, PhD; Christopher Pinard, DVM